Step Forward ServiceFamily and friends support group booklet
ContentsWhat is Step Forward?......................................................................\.......3The stages of change model..............................................\.......................5The role of trauma...........................................................\..............................6Supporting a loved one when they are struggling..........................................8Useful links for supporting a loved one who is struggling...............\...............9Practical support.......................................................\.....................................9The impact of stress.....................................................................\................12 Mental heath support for your loved ones................................\...................15
3What is Step Forward?At Step Forward, we offer psychological interventions and therapies to anyone over the age of 18 years who experience mental health difficulties.Due to Covid-19, we’ve adapted to a new way of working and are currently working virtually, most of the time.Our team is made up of Clinical Psychologists, Psychological Practitione\rs (nurses by background) and Assistant Psychologists.We do not have any Psychiatrists or medical doctors on the team (and therefore we cannot prescribe medication).As you can see from the diagram, we work with people who’s needs ‘fall between’ IAPT services and community mental health teams (CMHTs).Step forward is open Monday to Friday 9am to 5pm (excluding bank holidays). What to expect from therapy?What does the Step Forward Service offer to service users?Step Forward offers an initial assessment to discuss what service users are currently struggling with, their goals of therapy and to discuss what interventions Step Forward could offer.They will be offered to complete a safety document and psychoeducation sessions which include psychoeducation on mental health difficulties and discusses recovery from mental health difficulties.The next step could be an individual intervention, or a group intervention and a review will be offered to discuss the next steps.It is a normal part of the process to have breaks in between psychological interventions to consolidate what has been learned.GPIAPTservicesStep ForwardCMHTsWe’re here
4What does therapy involve?It’s a confidential space and what is talked about in the sessions will b\e kept private. However, if someone discloses risk to themselves or risk to others this information will need to be shared and confidentiality will be broken.It is time limited which means therapy will come to an end after a set number of sessions.At the moment, it is remote, and appointments are by telephone call or video call.Therapy is different from counselling sessions as there will be set number of sessions; there is a specific intervention; specific goals in mind and a specific aim of the sessions.When starting therapy, it is a normal part of the process for your loved ones to possibly feel worse (eg tired, low, or overwhelmed) as the sessions can be challenging and painful to begin with if it has brought up difficult feelings and memories.Your loved one may feel nervous about going back or want to quit but we would encourage them to try to stay with the process and talk about how they are finding therapy with their clinician. Their clinician will be happy to discuss this and will try to make adaptations if required or talk about how they can make the process as comfortable and easy to tolerate as possible.How you can help?It can be helpful for after the session to have something planned to enj\oy as a treat or something to help them relax.As friends and family, it may be helpful to talk to them about what they\
might find helpful from you as well, for example, would they appreciate spending time with someone, or planning something to look forward to together, or do they need a bit of time on their own to decompress. Either are completely fine and are expected, but it may be helpful to ask what they would prefer.
5The stages of change modelThe stages of change model can be useful to consider before making change or starting something new and can be applied to individual’s mental health recovery.Stage 1: Precontemplation. At this stage, there is no desire to make a change. You may feel unable or unwilling to change or feel hopeless or overwhelmed by the thought of change.Stage 2: Contemplation. At this stage, you can recognise that there are some problems, and you are ‘thinking’ of making change. You can notice some pros and cons of making change and might feel unsure or confused about making the change.Stage 3: Determination. At this stage, you believe that the benefits outweigh the negatives and start to take small steps towards change.Stage 4: Action. At the ‘action’ stage, you are actively doing something different and making the change. You are ‘moving forward.’Stage 5: Maintenance. You are sticking with the change over a period of time. New patterns of behaviour have been formed and are replacing the old ones.Stage 6: Relapse. This is when you fall back into old patterns of behaviour. It is normally accompanied with feelings of guilt, shame, disappointment and frustration. Relapse is a normal part the recovery process.Each stage is a normal part of the recovery journey in mental health. It is normal to feel at different stages at different points depending on what is happening in people’s lives. The stages do not necessarily go in order.Your loved one may struggle more at certain times and be more motivated at others depending on what stage they are on in the stages of change model.As family and friends, it’s normal for you to feel differently depending on what stage in the model your loved one is at, it could be frustrating or\
upsetting to see your loved one feeling less motivated or to seem them a\t the relapse stage.
6TraumaTrauma is something that occurs when individuals feel overwhelmed by something which is beyond their control.The events in our lives, especially in our childhood, have a big impact \on our mental health and wellbeing. Some of the most difficult experiences are called traumas. The more distressing and threatening the trauma is, the more likely it is that someone will experience some mental health difficulties either at that time or later in life.A trauma can be a one-off event such as an assault or a road traffic accident. It can also involve many events that have occurred over a long period of time. This is often called ‘complex trauma’. Not everyon\e realises the full impact on them at the time, and in fact sometimes peopl\e believe these experiences are normal, because they don’t know any different. However, we know that these traumatic events can have very severe consequences.Whether big or small, it can change how we view the world and respond or react to certain situations.Many people have never named the difficult experiences they have faced as ‘trauma’, and this may not be term they prefer to use. However, any experience that leaves you feeling overwhelmed, scared and alone can be traumatic, even if it doesn’t involve physical harm. If your survival, wellbeing, sense of yourself and of the future were threatened, then you experienced a trauma.Power threat meaning frameworkThe power threat meaning framework is used as an alternative approach to help us think about a person’s mental health difficulties rather than using a psychiatric diagnosis.A psychological formulation involves asking key questions such as:1. What has happened to you? For example, what life experiences have you been through?2. How did that affect you? For example, how did it make you feel when those things happened? What sense or meaning did I make of what happened to me? Did it make you feel; unsafe, afraid, attacked, rejected, helpless, powerless, controlled, bad, unworthy, excluded,
7alienated, alien, dangerous, contaminated, evil, failed, inferior, different, abnormal?3. How did you cope? For example, what behaviours or coping strategies did you learn to survive those experiences? Fight, flight, freeze, panic, phobias, flashbacks, suspicious thoughts, extreme moods, hallucinations, submitting, appeasing, striving, perfectionism, suicidal thoughts, and actions.Through asking these key questions, we can develop an understanding about ‘why’ a person may be struggling with their mental health.AttachmentThe four adult attachment styles
- A secure attachment style is low in both anxiety and avoidance. A Secure attachment tends to lead to stable and fulfilling relationship
- An anxious preoccupied attachment style is high in anxiety and low in avoidance. Anxious preoccupied attachments can create relationships that thrive on drama or are generally lower in trus
- A dismissive avoidant attachment style is low in anxiety and high in avoidance. This attachment style may lead to more distant relationships, sometimes stemming from a fear of commitmen
- A fearful avoidant attachment style is high in both anxiety and avoidance. People who display this attachment style are often drawn to close relationships, yet they are simultaneously fearful of them.Attachment styles are our way of interacting with and attaching ourselves to the people who are the most important to us. These styles influence our mindsets and behaviours in our closest relationships.These attachment styles start in childhood and continue in our adult life. They are not something that we typically talk or think about, but they can affect our lives in many ways.
8Emotional dysregulatio
- Emotional dysregulation is a term used to describe an emotional response that is poorly regulated and does not fall within the traditionally accepted range of emotional reactio
- When someone is experiencing emotional dysregulation, they may have angry outbursts, anxiety, depression, substance abuse, suicidal thoughts, self-harm, and other self-damaging behaviour
- Over time, this may interfere with someone’s quality of life, social interactions, and relationships at home, work, or schoo
- Changes in moods are often more intense and dramatic when people have faced difficult experiences in their lif
- When we were young, we may not have had the opportunity to learn how to manage or regulate emotions, and keeping feelings in balance may be very difficul
- Changes in feelings often have a trigger and often we don’t know what that is or where the next one will come fro
- Possible external triggers are events such as leaving home, starting college, having children, ending relationships and so o
- Our memories, thoughts or judgements may also be triggers, particularly if we are reminded of events or situations that were distressing or difficult.Supporting a loved one when they are struggling - safety plans at Step ForwardAt Step Forward, your loved ones will be offered to complete a written plan for them to keep, which provides the opportunity to talk about thoughts of harm or suicide which they may be experiencing, recognise possible triggers to these thoughts and identify ways of managing thoughts and support available around them to do this. Service users are invited to bring family members to safety planning sessions if they wish.What is in the safety plan?The safety plan involves discussing:
9Safety planWhat do I know about me? How will I know when I am at my best? How will I know when I am at my worst? What do other people notice?Suicidal thoughts and plansThis section is about learning as much as possible from current and previous suicidal thoughts and/or attempts, recognising potential triggers, past and present and to access personal strengths within the service user that has helped them come through difficult times. It is also intended to discover situations, moods and events that have been unbearable and have activated suicidal thoughts.Keeping the environment safeFor example, reducing access to medication and dangerous objects such as knives and razors. It can be difficult for your loved one to ask for help, though they will be encouraged to do this within safety planning session\s if they feel able to. Sometimes when people are struggling, they may find the presence of things like knives or medication comforting and may feel able to keep themselves safe without giving these items to others.Planning aheadThis section helps the service user identify triggers to difficult thoughts and to think through potential ways to manage this. If family members are involved, it can be helpful to get their perspective about possible triggers. If not at the sessions, service users are encouraged to have this conversation with family and friends and bring any more ideas to the next session.Building hopeThis involves identifying the service users’ strengths and creating goals for them to work towards. The hope box exercise teaches self soothing strategies and self compassion when individuals are struggling. This involves putting together items in one place which instil joy, calmness \and hope. Service users are asked to find items which stimulate their senses for example, soothing music (favourite uplifting song), smells (perfumes or candles), textures (favourite blanket or jumper), visual prompts (family/favourite photographs) and even tastes (favourite foods or snacks) an\d keep them together in one place to be accessed when they are feeling at their lowest. This can be a useful tool for family members to support th\eir loved ones to use when they are struggling.
10Reasons for livingThis supports the service user to identify reasons to carry on, to validate that this may feel difficult and that they are not alone in having to seek support.Emergency servicesThis highlights key individuals and services to access in an emergency. \This may include contact number for mental health services, family, and \friends as well as useful websites and online resources.Supporting a loved one when they are strugglingHow you can help your loved one
- Providing a loved one with space to talk about their feelings can be helpful. It isn’t necessary to provide answers or solutions, validating that things are difficult for them now can be enoug
- If you are worried that someone may be thinking about suicide, talk to them and ask them about how they are feelin
- Small gestures can be helpful, we don’t always need to talk directly about difficult thoughts if your loved one is not open to this. Providing opportunities to take their mind off distressing thoughts can be helpful. For example, by going for a walk together, watching tv together or going out for a coffee can distract and reduce the focus on thought
- Encourage them to seek treatment and support; it may be about attending therapy sessions, requesting a medication review from your GP or in urgent circumstances, seeking advice from urgent mental health support services or even A&E if you are worried that your loved one can’t keep themselves saf
- Offer practical support if things feel overwhelmin
- You can help them think of ideas for self hel
- You could direct them to their safety plan to use for support.
11Useful links for supporting a loved one who is strugglingSamaritans - www.
- Keep a diary for their appointments and meeting
- Keep a diary of medications and times they are to be taken, checking them off as they are take
- Know what benefits you may be entitled t
- Ask your local council’s social services department for a ‘carer’s assessment’. This assessment will see if you need any services to help you support someon
- See if there are any local services that can help you with practical support.
12Approaching challenging conversationsHere are some ideas of how to approach potentially challenging conversations with your loved ones
- Set time aside with no distraction
- Set the scene and have a specific topic in min
- Hold the conversation in a neutral space or give them a sense of contro
- Think about your own mindset before starting the conversatio
- Keep questions open ende
- Listen to what they are telling you and ask about their point of vie
- Agree how you will know if it is becoming too muc
- Come back to the topic later if things become heate
- It could be helpful to have a colour system to agree communication. For example: o Blue – I love you, but I need to be alone o Amber – I can’t talk, but I do need company o Red – I’m feeling angry and irritable, but it’s not because of you o Black – I’m feeling vulnerable today.The impact of stres
- It can be helpful to notice if how we are feeling ourselves is impacting on how we relate to others at that moment in time (if it is an especially stressful time, it might not be the best time to have challenging conversations or it might be helpful to make some time to look after ourselves first
- We can’t support someone to the best of our ability if we don’t also make time to take care of ourselves.
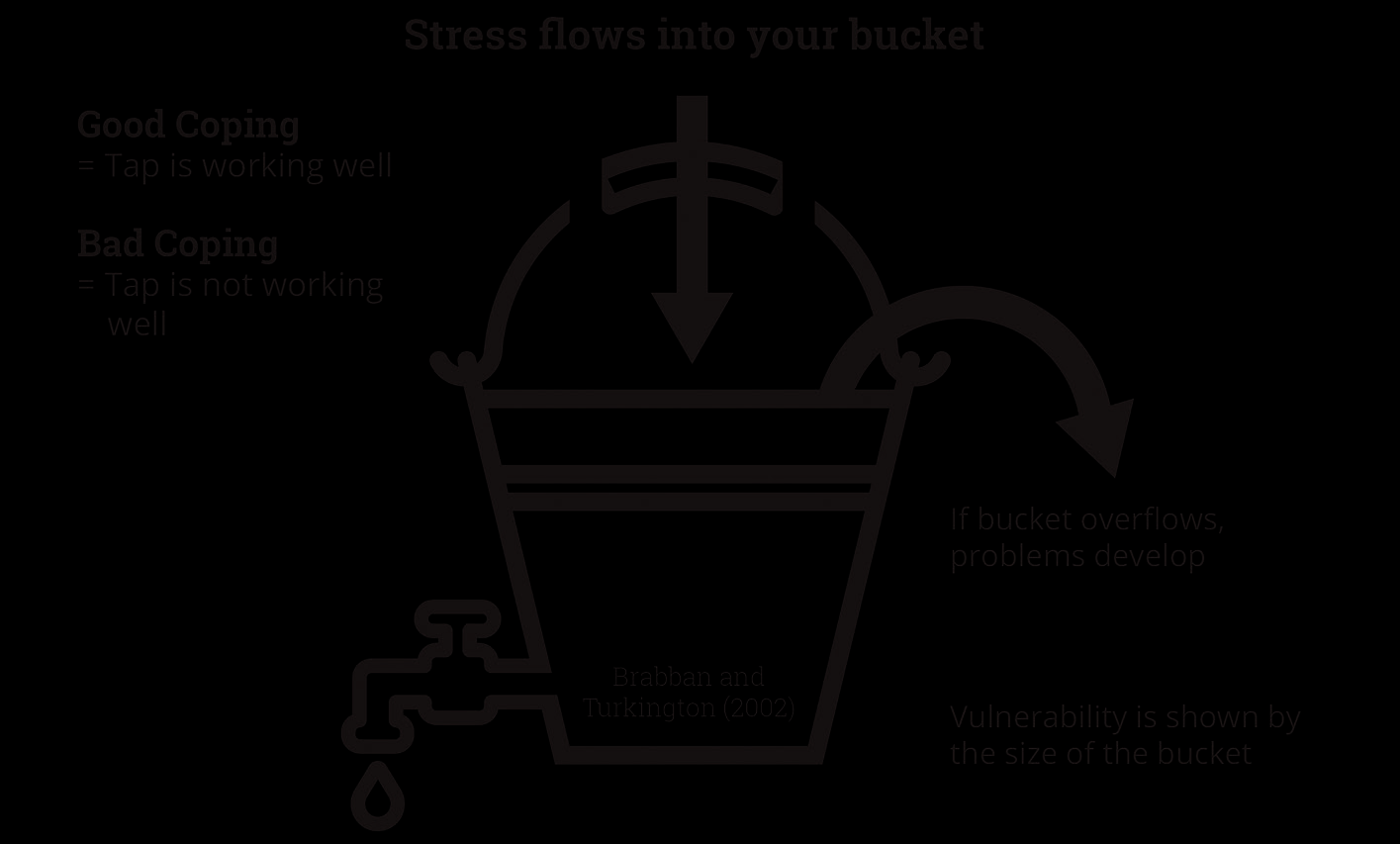
13The stress bucketEvery one of us has some degree of vulnerability that would put us at risk of developing a mental health difficulty. For example, trauma, abuse, loss, social isolation, poverty, neglect, genetics, family history, etc
- All of us would at some point experience being exposed to some stressor, for example, loss, illness or relationship difficultie
- People with more vulnerability factors may be more at risk of developing mental health difficulties when exposed to lower levels of stress than someone who has fewer vulnerability factor
- However everybody, if they had enough stress in their lives, would experience mental health difficulties, even if their vulnerability is lo
- Our vulnerability is the size of bucket, stress flows into the bucket and if the bucket overflows, we may develop mental health difficultie
- Different stresses can make our bucket fill up including challenging conversations or worrying about your loved one
- If the tap is working someone is coping well and this helps release water from your bucket and prevents it from overflowin
- If the tap is not working someone is not coping well so water fills th\e bucket and it overflows.
14Looking after ourselve
- We all need a balance of pleasure, mastery, and necessary (routine) task
- Pleasurable activities – things we usually find enjoyable or fu
- Mastery activities – things that make us feel like we have achieved somethin
- Routine or necessary activities – things that must be done (or otherwise there will be negative consequences, like taking medication) or that we do at set times in the day (like brushing teeth\
or mealtimes
- We need a balance of these activities every day, so we have had the chance to have some enjoyment, as well as to feel we have achieved things we wanted t
- When we are supporting somebody else who is having a difficult time, we may find these become out of balance, or we lose one type of activity, our sense of routine may be hard to keep up with, or we lose time for pleasurable activities for ourselve
- It is important to make time for all of these things and to keep a sense of balance between each type of task. If we focus more on one type of task, we may notice a dip in our mood or feel out of control
- If things feel out of balance, it can be helpful to try to plan our days\ in advance and try to keep to this schedule (as we’re more likely to make time to things and stick to it if we have planned in advance
- When you start this, it might be helpful to notice how much of a sense of pleasure and achievement tasks bring you, and perhaps try out some different things if needed.
15Mental heath support for your loved onesStep Forward is unable to provide crisis support and unable to provide general mental health support outside of routine appointments. However, there are a number of services which can provide immediate responses.Immediate mental health supportMersey care urgent mental health support line: 0800 145 6570For urgent mental health support If your loved one in a crisis and there are risks to their safety and wellbeing. This number is available 24/7.Shout text service: Text HEAL to 85258 Free, confidential, 24/7 text message support is available if someone is feeling overwhelmed or struggling to cope.General mental health supportSamaritans: For general support, call 116 123 or for 24-hour crisis support, call 01517088888. You can also email jo
to 45 minutes and is free. Available 10am to 4pm, Monday to Thursday. Please call to book on 01517071826.Papyrus HOPELINEUK: Call: 08000684141 or text: 07860039967 or email: pat
For children and young people under the age of 35 who are experiencing thoughts of suicide and for anyone concerned that a young person could be thinking about suicide.Opening hours for 9am to midnight every day of the year (weekends and Bank Holidays included).
Support services and information for family and friendsLocal solutions: www.
Sefton Council: www.